Abstract
Peripheral blood stem cell (PBSC) mobilisation in multiple myeloma (MM) patients after exposure to daratumumab (D), a CD38 targeting monoclonal antibody, produces a lower stem cell yield possibly due to an effect on CD34+ stem cells (Hulin et al., 2021). Similarly, the GRIFFIN study reported greater plerixafor usage to facilitate PBSC mobilisation in patients randomised to DARA-Velcade, Lenalidomide and Dexamethasone (D-VRd) when compared to VRd (Voorhees et al., 2020). In addition, R use has previously been shown to impact adversely on PBSC yields (Kumar et al., 2007) with a recommendation to use cyclophosphamide (cyclo) assisted mobilisation for this group of patients (Mazumder et al., 2008). In this context there remains uncertainty about the role of plerixafor, compared to chemotherapy assisted mobilisation.
Aim: To investigate the effect of DRd on PBSC mobilisation and to determine the outcomes of G-CSF (G) + cyclo and G +/-plerixafor mobilisation for patients with prior DRd exposure and to compare PBSC yields to patients mobilised after Velcade, Cyclophosphamide, Dexamethasone (VCD) based induction therapy
Methods: The ALLG MM21 study (ACTRN12618001490268) is a multicentre study of transplant eligible refractory and/or relapsed MM patients. Patients were eligible if they had progressive disease or less than a partial response to prior VCD induction therapy. D at 16mg/m2 and d at 40mg was administered on Day 1,8,15 and 22 in combination with R 25mg D1-21 for the first 2 induction cycles. From cycle 3, D was administered fortnightly with R 10mg D1-28 and d 40mg weekly. PBSC mobilisation was undertaken after 2-3 cycles of DRd with a minimum of 14 days off R and D prior to proceeding. The PBSC mobilisation approach and the need plerixafor were based on institutional practice.
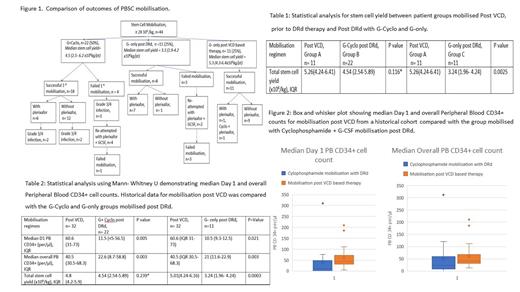
Results: Fifty patients were enrolled on trial. Three patients experienced progressive disease and 3 patients died prior to mobilisation. A total of 44 patients underwent PBSC mobilisation,11 (25%) of these post-VCD but prior to starting DRd received G-only (Group A); 22/44 (50%) post-DRd received G + cyclo (Group B); and 11/44 (25%) post-DRd received G-only (Group C) (Figure 1). Based on low day 1 CD34+ counts 13/33 (33%) patients required plerixafor post-DRd and 2/11 (18%) post-VCD. Post-DRd 7/33 (21%) patients failed to collect more than 2 million cells/kg and 4 then failed a second attempt at mobilisation. All patients post-VCD/pre-DRd were successfully mobilised. Total PBSC yields were comparable between Groups A and B but significantly lower for Group C versus Group A (Table 1). Group B patients were then compared to a contemporaneous group of non-trial VCD treated and G only mobilised patients (n = 32) and found to have significantly inferior day 1 median peripheral blood (PB) CD34+ cell counts (Table 2, Figure 1). Seven patients (21%) who received G + cyclo experienced grade 3/4 infections with 5 of the 7 demonstrating day 1 PB CD34+ cell counts of <5 per/µl. There were more apheresis days with median 2.5 days (1-5) in the G+ cyclo (Group B) compared to the other G-only or G+ plerixafor groups (median 2 days (1-3)).
Conclusions: PBSC collection after DRd salvage was characterised by lower CD34+ cell mobilisation and lower overall PB CD34+ yields when compared to patients mobilised after receiving VCD. Cyclo assisted mobilisation but not G + plerixafor abrogated this effect. Further evaluation of strategies to mitigate against the impact of DR containing induction are required.
Indran: Jansse-Cilag Pty Ltd.: Other: Registration costs , Patents & Royalties. Quach: Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Karyopharm: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; GlaxoSmithKline: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen/Cilag: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Antengene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; CSL: Consultancy, Membership on an entity's Board of Directors or advisory committees. Janowski: BMS/Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen-Cilag: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Regeneron: Membership on an entity's Board of Directors or advisory committees; Astrazeneca: Membership on an entity's Board of Directors or advisory committees. Estell: Celgene: Membership on an entity's Board of Directors or advisory committees; Janssen-Cilag: Membership on an entity's Board of Directors or advisory committees. Spencer: Celgene: Honoraria, Research Funding, Speakers Bureau; Janssen-Cilag: Honoraria, Research Funding, Speakers Bureau; Amgen: Honoraria, Research Funding; BMS: Research Funding; Takeda: Honoraria, Research Funding, Speakers Bureau; STA: Honoraria.
The combination of Daratumumab, Lenalidomide and Dexamethasone therapy is not approved on the Pharmaceutical Benefits Scheme in Australia.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal